Metastatic Lobular Breast Cancer
Invasive lobular carcinoma (ILC) is a distinct subtype of breast cancer with unique cellular structures, biology, and behavior. ILC is the 2nd most common type of breast cancer and accounts for up to 15% of all breast cancers including mixed ductal /lobular. 90% of lobular breast cancers are ER/PR+ HER2-, although there are subpopulations that are ER/PR negative, triple negative, or HER2+. This histology can also change over time due to treatment resistance and acquired genomic mutations. In addition to the most common type of Classic ILC, there are special morphological subtypes including Pleomorphic, Solid, Alveolar, and Tubulo-lobular which have different characteristics.
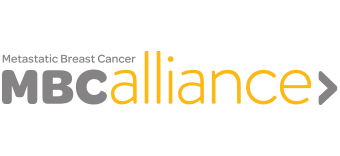
ILC differs from invasive ductal carcinoma (IDC) in that the cells grow in a single file and do not always form a lump or a mass and therefore can be harder to diagnose. ILC has frequent late recurrences and is generally slow growing. Because of ILC’s unique features there are challenges in initial diagnosis, imaging for staging, and clinical trial enrollment. Importantly, metastatic ILC can travel to unusual sites.
Currently treatment is the same for ILC as IDC , depending on histological subtype. In early stage ILC, studies have shown some evidence that ILC may respond differently than IDC to Tamoxifen and Chemotherapy. Two recent reviews on metastatic breast cancer have shown that CDK4/6 inhibitors and Erubulin (a single agent chemotherapy) show similar efficacy in metastatic ILC when compared to IDC.
ILC has not yet been studied enough to be well understood and more research is needed to refine treatments for people living with metastatic ILC.
This month’s content was developed in collaboration with the Lobular Breast Cancer Alliance (LBCA). The LBCA was founded by patients to raise awareness about ILC and stimulate more ILC research. Their website provides the most current information about ILC and metastatic ILC and houses a comprehensive ILC publications library. Learn more about ILC and the LBCA at https://lobularbreastcancer.org.
Click on the image in each section below to read more about the science behind the topic.