Breast Cancer Brain Metastasis
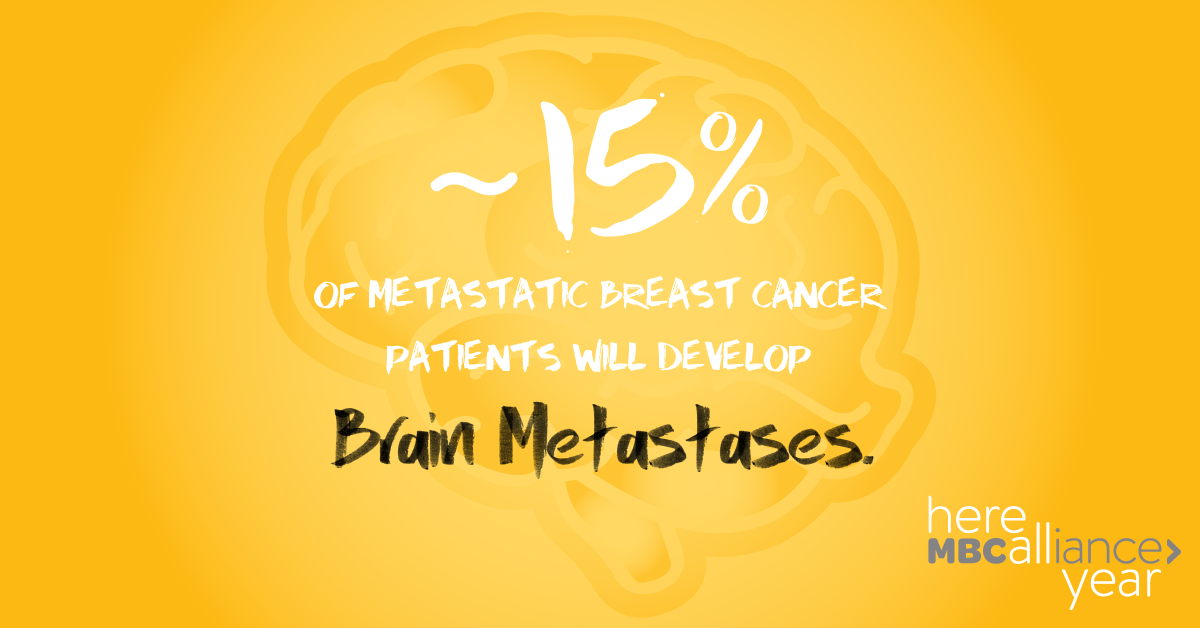
When breast cancer spreads from the breast to other parts of the body, it is termed “metastatic.” The most common sites of spread in breast cancer are the bones, liver, lungs, and brain. At a metastatic diagnosis, doctors commonly scan the body for signs of spread, but most patients do not receive a brain scan unless they have symptoms like numbness or headaches. This month, the Metastatic Breast Cancer (MBC) Alliance is focusing on breast cancer brain metastasis. The incidence of brain metastasis is growing as new therapies help patients live longer with MBC. As in all things MBC, we need more research, earlier screening, and scientific breakthroughs. For a patient living with breast cancer brain mets, the need for research is enormous and HERE ALL YEAR.